Your Cornea
You will be undergoing an operation to repair an important part of your eye called the cornea. The cornea is the clear, circular, protruding portion of your eye often referred to as the “window” of the eye. The cornea must remain transparent in order to have good vision. Disease and trauma can reduce this brilliant clarity, resulting in visual loss. The cornea has an outer layer, the epithelium, which serves as a boundary against infection. Under the epithelium is the stroma, which is a collagen layer that comprises the majority of the cornea. On the inner surface, there is a layer of cells called the endothelium. We will discuss your particular condition, the reason for your visual loss, and the specific type of surgery we recommend.
Obtaining a Donor Cornea from the Eye Bank
Transplanted corneas come from a donor who has willed his or her cornea(s) for transplantation, or whose family has donated the cornea after the donor’s death. It may be upsetting to look at the deceased person as a source of replacement tissue, but for most families, the opportunity to give sight to another person is comforting.
When we determine that you would benefit from a corneal transplant, we will contact the Eye Bank and place you on the waiting list. All corneas are screened for HIV, hepatitis, and other infectious diseases.
The waiting period is usually about four to six weeks. You will be tentatively scheduled at the hospital or ambulatory surgery center with an operating date. Usually, a cornea is available on your scheduled date. If one is not available, your surgery will be rescheduled soon after the original date.
Partial Thickness Corneal Transplant (Endothelial Keratoplasty) vs. Full Thickness Corneal Transplant (Penetrating Keratoplasty)
Until 2006, full thickness (replacing all of the layers of the cornea) corneal transplants had been the standard of care for patients requiring corneal transplantation. Recently, corneal specialists have been able to target replacement of just the diseased endothelial (inner) layer of the cornea. In DSAEK (Descemet’s Stripping Automated Endothelial Keratoplasty) procedures the inner portion of the cornea is replaced. In DMEK (Descemet’s Membrane Endothelial Keratoplasty) only Descemet’s membrane, the innermost layer, is replaced. You have been offered the partial thickness procedure because the endothelial layer of your cornea, which rests on the Descemet’s membrane, is not working properly, causing your cornea to swell.
The replacement is done through a small incision at the edge of the cornea to minimize changes to the front surface of the cornea. By minimizing the number of sutures (usually one to three) and by using a small incision, there is quicker healing and faster recovery time as well as less induced astigmatism (or corneal irregularity).
Since fewer sutures are used during an Endothelial Keratoplasty, an air bubble is placed in the eye to hold the donor cornea in place. You will be asked to lie on your back for a few days (except to use the bathroom, eat or visit us) to allow the new cornea to attach and adhere to your cornea.
A full thickness corneal transplant patient might take a year or so to heal. In comparison, patients undergoing an Endothelial Keratoplasty usually recover good vision within a few months or possibly weeks.
Since there is a smaller incision and fewer sutures in the front part of the cornea, there is less risk of wound rupture or discomfort from broken or loose sutures. The corneal shape is also more stable earlier in the post-operative period. In addition, there is an advantage to introducing a thinner layer of foreign tissue into the body – decreased risk of corneal rejection.
Since the recovery period is much quicker with Endothelial Keratoplasties than with full thickness corneal transplants, patients with bilateral corneal disease can be considered for treatment of the second eye much more quickly to achieve better vision in both eyes.
Before Your Surgery
Blood samples, EKG, and/or chest X-rays may be required depending upon your age and health status.
On the day before surgery, our office will call you to let you know if an appropriate donor has been found. In addition, a nurse from the hospital or ambulatory surgery center will call you in the late afternoon or early evening to let you know what time to arrive for your surgery.
On the Day of Surgery
Plan on being at the hospital or ambulatory surgery center for about 5 hours. Surgery is usually done on an outpatient basis. You must have an accompanying person who will take you home.
1. Do not eat or drink anything after midnight on the night before surgery.
2. When you come for surgery, please bring all your medications in their original labeled bottles. Also, provide information on any known allergies.
3. A nurse will ask you about your general state of health. Later, an anesthesiologist will screen you prior to surgery (most corneal transplants are done under local anesthesia).
4. Eye drops, including antibiotics, will be administered.
During Your Surgery
• If you are having local anesthesia:
a. The physician will inject medication around your eye
to temporarily prevent pain and movement. The medication will also block your vision during surgery.
b. Sterile drapes will be placed to isolate the eye having
the surgery. Adequate ventilation will be provided.
c. Inform the physician or the nurse if you happen to feel any pain or become nauseated during surgery.
• If you are having general anesthesia (less common):
a. You will wake up in the recovery room.
b. You will be returned to your room usually after about
one hour in the recovery room.
• A protective shield will be placed over your operated eye when surgery is complete. You will be asked to stay on your back facing the ceiling.
After Your Surgery
1. You will be asked to stay in the hospital for an hour or two after your surgery. You will then be examined. At that time, some air may be released from the eye or additional air may be placed. If necessary, you may walk to the bathroom with the assistance of the nursing personnel and you may elevate the head of your bed for meals. You will be asked to lie on your back looking up towards the ceiling for the first few days to allow the transplanted cornea to remain in its proper position. Exceptions include going to the bathroom, eating and coming for follow-up appointments.
2. If you had local anesthesia, you may resume your regular diet. If you had general anesthesia, liquids will be given for your first meal. You may resume your regular diet the following day.
3. The eye dressing will remain in place until the morning following the surgery when you will have your first post-operative appointment. If you can open your eye under the patch, try to keep it closed.
4. After the doctor removes your eye shield the next morning, your eye will be examined. Antibiotic, dilating and steroid drops will be instilled to prevent infection and rejection of the donor cornea. You should wear glasses during the day and a shield at night. You must wear one or the other at all times for four weeks. DO NOT RUB OR SCRATCH YOUR EYE.
5. Eye pain following a corneal transplant is usually minimal. Let us know if you have sudden, severe, and/or persistent pain.
Instructions for Home Care
1. You will probably be discharged on the day of surgery.
2. Antibiotic and dilating drops will be prescribed for one month. Steroid drops will be prescribed for at least one year.
3. If you do not have enough eye medication at home, call us at (212) 305-3378 or (914) 723-1641 with the name of the medication and the phone number of your pharmacy. It is crucial that you receive every dose of your medication. Please plan ahead if you see that your drops are running low. Try not to run out in the evening, on the weekend or during a holiday!
4. You may clean around your eye, but do not rub the eye. If there is crusting, use a clean, wet washcloth to gently wipe the eye once or twice a day. Never put the washcloth into the eye or use the same part of the washcloth twice. Avoid pressure on the eye.
5. Over the following weeks, you should avoid strenuous activity that causes you to become red in the face, as straining increases pressure in the eye. If it is necessary to cough or sneeze, do so with your mouth open. Do not lift, push, or bend with your head lower than your heart.
The instructions below are to be followed unless your physician informs you otherwise:
After Two Days You May:
– Read or watch TV until your eye becomes tired (the day after your surgery)
– Return to school or work if it does not involve strenuous activity or lifting
– Drive a car if the corrected vision in your unoperated eye is 20/40 or better
– Shower if you prevent soap from getting into your eye (usually about 2 days after surgery)
– Shampoo your hair with your head tilted backwards (usually about 2 days after surgery)
– Do light housework
You may NOT:
– Participate in sports until approved
– Strain or lift (any activity which may cause your face to redden)
– Bend over with your head lower than your heart
Risks of Endothelial Keratoplasties
I. Risks Similar to Full Thickness Corneal Transplants
There may be mild pain, redness, stinging and/or itching for one week after surgery that usually responds to Tylenol. Serious infections or bleeding may occur in 1 out of 1000 patients. There is also a risk of developing high pressure (glaucoma). Usually, this is controlled with eye drops.
There is a good chance that your corneal transplant will be successful. If it fails, it will most likely fail because your body recognizes the new corneal tissue as foreign and tries to reject it. This can occur at any time (even years after the surgery). Rejection can result in a cloudy corneal transplant which may require a repeat corneal transplant. The body attempts to reject the full corneal transplant in about 20% of cases, a DSAEK in about 2-3% of cases, and likely even less in DMEK.
If the transplant rejection is treated early in its course, 90% of the time it can be reversed with medications, usually just topically, and the corneal tissue will again be clear. In cases where the rejection is not treated early in the course, the chance of eventual corneal transplant failure is much higher. Therefore, it is extremely important for you to recognize the signs of impending corneal transplant rejection and to report them to us as early as possible.
If any of the following danger signs persist for 24 hours, call the office at (212) 305-3378 or (914) 723-1641.
1. Decreased Vision – the most common way that you may notice early corneal transplant rejection is by a decrease in vision.
2. Increased Pain – after surgery, there may be some discomfort around the eye, but this should go away in a few days. If the eye becomes increasingly uncomfortable, it could be a sign of a corneal transplant rejection or infection.
3. Increased Redness – after surgery, there may be some redness or swelling. It should slowly start improving within a few days. If instead the eye is getting more red or more swollen, please call.
4. Increased Light Sensitivity – After surgery, your eye(s) may be light sensitive. You will be given dark glasses to wear. The light sensitivity should slowly diminish over a few days or sometimes weeks. If it should worsen or recur once it has been resolved, please call.
Flu shots: at times, this vaccination may increase the risk of rejection. If you plan on getting a flu shot before surgery or any time after surgery, please notify us. Sometimes drops will be prescribed before you receive the flu shot.
Note: Corneal transplant rejection can occur at any time (even years) after surgery. Again, it is important to remember that rejections can be reversed if caught early so make sure you see an ophthalmologist soon after any of the above symptoms (preferably within a day or two).
II. Risks Unique to Endothelial Keratoplasties
During the surgery, your doctor may find that it is not possible to continue or complete the partial thickness transplant surgery safely. Because safety of your eye is the highest priority, your doctor may decide to change the surgery to a standard full thickness transplant or even halt the surgery and reschedule it with new donor tissue.
After the surgery, dislocation of the partial thickness corneal transplant tissue within the eye is possible early in the post-operative period (days to weeks). This would require repositioning of the tissue under local anesthesia (either in the office or operating room). If the tissue can not be repositioned, a repeat partial thickness or full thickness corneal transplant might be offered.
Administering Ophthalmic Drops or Ointments Dosage:
Always follow the directions given to you by your physician. Do not skip doses and never use the medication more often or longer than prescribed. Make sure you do not run out of your medications.
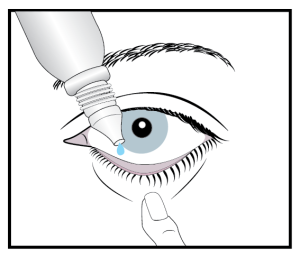
How to Administer Drops:
1. Wash hands thoroughly.2. If the bottle has been in the refrigerator, warm it by gently rolling it between the palms of your hands.3. Shake bottle as directed.4. Apply one drop inside the lower pocket of the eye formed when the lid is pulled down (see illustration). |
|